Authors: Silvio Giannetti, Nicola Bizzotto, Andrea Stancati, Giuseppe Orlando, Attilio Santucci.
Abstract
Isolated radial neck fractures are very rare and the majority can be treated conservatively. However, conservative treatment might result in malunion and/or secondary displacement. The open reduction and internal fixation (ORIF) is not free from complications such as screw or plate dislocation, failure of the implant and infections.
A middle way between the two approaches could be represented by the closed reduction technique using intramedullary stabilization. The purpose of this study is therefore to evaluate the functional outcome of radial neck fractures treated by intramedullary reduction and stabilization with k-wire.
Introduction
Radial head and neck fractures are the most common fractures of the elbow but in adults isolated radial neck fractures are very rare with an incidence of 1 % of all fractures [1,2]. The goals of treatment are to restore elbow stability, maintain the relative length of the radius, and preserve elbow function.
The treatment of these fractures in adults consist of either conservative management, open reduction and internal fixation (ORIF), excision of the radial head, or radial head arthroplasty [3].
Displaced and angulate radial neck fractures are usually treated with an open reduction and internal fixation method in adults [4] while the closed intramedullary pinning is often used for the reduction and fixation of displaced radial neck fractures in children [5, 6].
The current authors report the mid-term results of a minimally invasive tech¬nique in adults with closed reduction and internal fixation with retrograde intramedullary wires being introduced from the distal portion of the radius.
This technique results in anatomical reduction of displaced neck fractures, less pain along the forearm, no disturbances at the distal radioulnar joint, faster rehabilitation, and easier hardware removal after complete fracture consolidation.
Materials and methods
Between February 2011 and June 2016, a total of 15 patients were treated with closed reduction and intramedullary osteosynthesis. All patients had suffered from an isolated radial neck fracture without clinical joint instability (type II or III fractures according to Mason’s classification [7]). Nine patients, were diagnosed with Mason type II fracture and six patients with Mason type III fracture.
In our record 10 males and 5 females were included in the study, with a mean age of 32 years (22-45 years).
Six patients had injuries on the left upper limbs and nine on the right. The mean time from injury to the surgery was 2,2 days (range 1-5 days).
With a mean of 28 months (range 6–43 months; minimum 6 months) all patients returned for the follow-up survey.
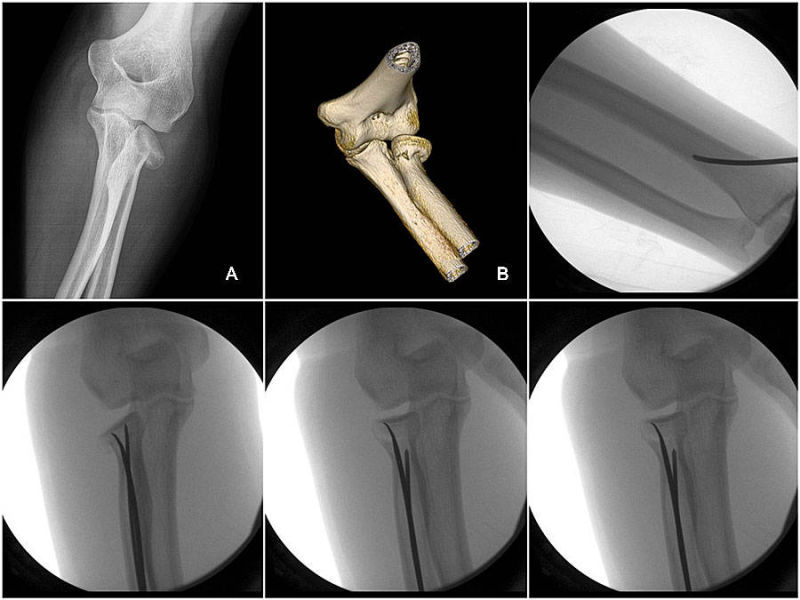
Clinical and radiological examina¬tions (Fig. 1) were performed by the authors specifically for this study.
Objective assessment consisted of a physical examination for active elbow range of motion (ROM) for flexion/extension and pronation/supination as well as forearm rotation of both the injured and the contralateral arm.
For subjective evaluation, patients filled in the Elbow Self Assessment Score form (ESAS) [8]. A functional score was collected using the form of Mayo Elbow Performance Score (MEPS) and the Disabilities of the Arm, Shoulder and Hand (DASH) Score.
Postoperative X-rays were evaluated for bone healing, heterotopic ossifications and the alignment of the radio-capitellar joint.
Surgical technique
All patients underwent sur¬gery, performed by the same surgeon (A. Santucci), at the authors’ institution. The repair was performed under regional an¬esthesia. Patients were placed supine with the injured arm on a radiolucent table. A preliminary reduction was performed by direct external maneuvers on fracture site associated with pronation and supination maneuvers of the wrist.
As entry point for the K-wire, the metaphyseal zone of the styloid process of the distal radius was identified under image intensifier (Fig. 2). The radial neck fracture was stabilized by passing one or two intra-medullary retrograde K-wires into the radial head and then by performing the “joystick technique” the fragments were reduced into the anatomic position (Fig 3). No additional surgical procedures were necessary in any case.
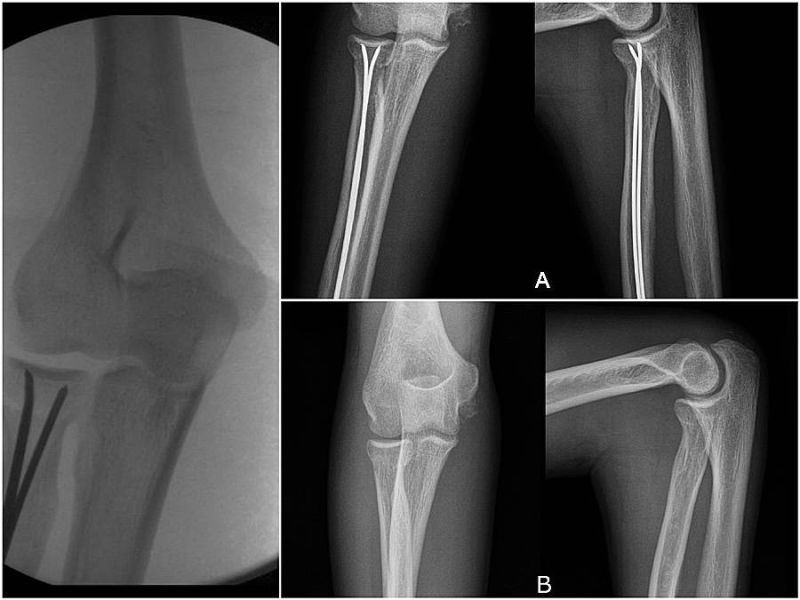
As postoperative management, all patients were immobilized with a plaster cast for 10 days and after they began the gradual recovery with an articulated joint brace. The K-wire removal was performed after 40 days (Fig. 4). Sporting activities were restricted for 3 months.
Statistical Analysis
Student’s t test and analysis of variance were used to analyze the data. For power analysis, the alpha error was set at 5% (95% confidence interval) with a level of significance of P<.05.
Results
Clinical examination showed satisfactory outcomes in all patients. There was no nerve injury at wound site, no infection, no increased varus or valgus deformity of the operated elbow . ROM side-to-side was complete in 14 cases, of extension and flexion as well as of forearm rotation. At final follow-up, in 1 patient a limitation of flexion of less than 10° was observed.
As functional scoring, the MEPS score was 95.11 ± 6.98 (range 84–100) (P<.012) representing nine good and six excellent results and the DASH score revealed good to excellent outcomes with 6.32 ± 10.24 points (range 0–28) (P<.019). The ESAS score was 98.35 ± 1.89 (range 94–100) (P<.015) indicating a non-restricted elbow function. At final follow-up observation, acceptable radiographic reduction was achieved, the angulation was less than 10° and displacement was less than 2 mm. In all cases no heterotopic ossifications were observed and bone union was present at 12 weeks from post operation.
Discussion
In the last few years an open surgery approach has become widely accepted to treat Mason type II or III fractures [9, 10]. However some studies suggest that operative treatment has no major advantages compared to conservative methods. [11,12,13,14]. In the Lindenhovius et al. study [15] the authors, after plate and screws fixation of isolated Mason type II fracture, underline that the outcomes are comparable to the ones achieved by conservative means in prior investigations [11, 14].
However some authors believe that there may be an indication for the closed reduction and intramedullary stabilization especially in those cases where the ORIF procedure might be considered an overtreatment and the conservative treatment might just not be enough [16].
The advantages of a minimally-invasive technique consist in the avoidance of implant—related complications (screw or plate dislocation, rupture) affecting the proximal radio-ulnar joint.
In addition, the ORIF is associated with a higher rate of avascular necrosis [17], heterotopic ossifications [18], proximal synostosis [19], infections and loss of ROM [18].
However the technique described in this paper is not free of potential complications and special attention has to be taken to avoid superficial radial nerve's injuries [16]. In addition, a second surgery is necessary for the removal of the stabilization's instrumentation.
In case of type III Mason fractures, there are different treatment options mentioned in the literature: reconstruction techniques, radial head removal [14] or radial head replacement [20]. Ring et al. conducted a study to evaluate the functional results of the ORIF treatment of radial head fractures and concluded that it should by recommended to replace the radial head, rather than repair it, in patients with comminuted fractures with more than three fragments. [21].
There are few studies in the literature concerning closed reduction and internal fixation of the radial head and neck fractures in adults. Sandmann et al. [16] and Strychar et al. [22] have described good functional results and a very low complications rate of radial neck fractures (Mason II and III) in adults treated by closed reduction and internal fixation with K-wire or TEN.
Also in our study we have obtained good to excellent functional results with no complications and a faster return to sports activities.
From our point of view, the strengths of this method are: 1) possibility of reducing the fracture anatomically, percutaneously, therefore without the need to perform any arthrotomy; 2) possibility of obtaining a stable osteosynthesis, in order to grant an early mobilization of the limb during the consolidation phase of the fracture; 3) the hardware removal can be performed more easily when the movement's recovery is completed and the consolidation of the fracture is at an advanced state.
However, we believe that a randomized controlled trial with a long-term follow-up may provide further guidelines for the optimal management of these fracture types.
Conclusion
Our good to excellent functional results, without affecting the elbow range of motion or patients’ activities of daily life, support the statement that this approach, as described by Judet in children [5], can also be an alternative surgical procedure in the treatment of displaced radial neck fractures (Mason II and III) in adults.
Figures
Fig. 1: Pre-operative X-Ray (A) and CT-scan (B)
Fig. 2: entry point for the K-wire
Fig. 3: intraopera¬tive intensifier control
Fig. 4: A) post-operative X-ray (AP and LL). B) X-ray control after the hardware removal
References
1. L. Kaas, R.P. Van Riet, J. Vroemen, The epidemiology of radial head fractures. J Shoulder Elbow Surg. 2010, 19(4):520-3.
2. A.D. Duckworth, N.D. Clement, P.J. Jenkins, S.A. Aitken, C.M. Court-Brown, M.M. McQueen, The epidemiology of radial head and neck fractures. J Hand Surg Am. 2012;37(1):112–9.
3. J. Zwingmann, M. Welzel, D. Dovi-Akue, H. Schmal, N.P. Südkamp, P.C. Strohm, Clinical results after different operative tre¬atment methods of radial head and neck fractures: A systematic review and meta-analysis of clinical outcome. Injury, 2013, 44(11), 1540-1550.
4. Burkhart KJ, Gruszka D, Frohn S, Wegmann K, Rommens PM, Eicker CM, Muller LP. Locking plate osteosynthesis of the radial head fractures: clinical and radiological results. Unfallchirurg. 2015;118(11):949–56.
5. M Judet H, Judet J. Fractures and orthopedicque de l´enfant. Paris: Maloine; 1974. p. 31–9.
6. Metaizeau JP, Laskombes P, Lemelle JL. Reduction and fixation of di¬splaced radial neck fractures by closed intramedullary pinning. J Pe¬diatr Orthop 1993;13:355-359.
7. Mason ML. Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg 1954; 42:123-132.
8. Beirer M, Friese F, Lenich A, Crönlein M, Sandmann GH, Biberthaler P, Kirchhoff C, Siebenlist S. The Elbow Self-Assessment Score (ESAS): development and validation of a new patient-reported outcome measurement tool for elbow disorders. Knee Surg Sports Traumatol Arthrosc. 2015.
9. Boulas HJ, Morrey BF. Biomechanical evaluation of the elbow follo¬wing radial head fracture. Ann Hand Upper Limb Surg 1998;12:314- 320.
10. Van Glabbeek F, van Riet R, Verstreken J Current concepts in the treat¬ment of radial head fractures in the adult: a clinical and biomechanical approach. 2001 Acta Orthop Belg 67:430-441.
11. Weseley MS, Barenfeld PA, Eisenstein AL. Closed treatment of isolated radial head fractures. J Trauma. 1983;23:36 –39
12. Lindenhovius A. et al. The Long-Term Outcome of Open Reduction and Internal Fixation of Stable Displaced Isolated Partial Articular Fractures of the Radial Head. The Journal of Trauma Injury, Infection, and Critical Care. Volume 67, Number 1, July 2009.
13. Frankle MA, Koval KJ, Sanders RW, Zuckerman JD. Radial head fractures associated with elbow dislocations treated by immedia¬te stabilization and early motion. J Shoulder Elbow Surg. 1999 Jul- Aug;8(4):355-60.
14. Herbertsson P, Josefsson P O, Hasserius R, Besjakov J, Nyqvist F, Karls¬son M K. Fractures of the radial head treated with radial head excision. J Bone Joint Surg (Am) 2004; 86 (9): 1925-30.
15. Lindenhovius A. et al. The Long-Term Outcome of Open Reduction and Internal Fixation of Stable Displaced Isolated Partial Articular Fractures of the Radial Head. The Journal of Trauma Injury, Infection, and Critical Care. Volume 67, Number 1, July 2009.
16. Sandmann GH, Crönlein M, Neumaier M, Beirer M, Buchholz A, Stöckle U, Biberthaler P, Siebenlist S. Reduction and stabilization of radial neck fractures by intramedullary pinning:a technique not only for children. Eur J Med Res (2016) 21:15
17. Girard JY, Rogez JM, Robert R, Leborgne J. Vascularisation of the head of the radius in the adult. Surg Radiol Anat. 1995;17(1):41–5.
18. Foruria AM, Augustin S, Morrey BF, Sanchez-Sotelo J. Heterotopic ossification after surgery for fractures and fracture-dislocations involving the proximal aspect of the radius or ulna. J Bone Joint Surg Am. 2013;95(10):e66.
19. Jupiter JB, Ring D. Operative treatment of post-traumatic proximal radioulnar synostosis. J Bone Joint Surg Am. 1998;80(2):248–57.
20. Prosthesis replacement in Mason III radial head fractures: A meta-analysis. Dou Q, Yin Z, Sun L, Feng X. Orthop Traumatol Surg Res. 2015 Oct;101(6):729-34.
21. Ring D. Quintero J. Jupiter J. Open Reduction and Internal Fixation of Fractures of the Radial Head. Journal of Bone and Joint Surgery; Oct 2002; 84, 10.
22. Keller HW, Rehm KE, Helling J. Intramedullary reduction and stabilisation of adult radial neck fractures. J Bone Joint Surg Br. 1994 May;76(3):406-8.
SHARE THIS PAGE!